A staggering 15.6 million adults in the United States reportedly used at least one botanical supplement with potential hepatotoxic effects within the last 30 days, according to an in-depth survey study that utilized data representative of the national demographic.
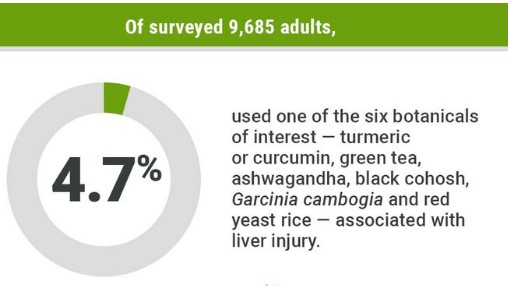
In this study, where more than 9,600 users of NHANES were sampled, the overall prevalence of herbal and dietary supplement use was assessed at 57.6%. Among them, 4.7% of respondents reported using six botanicals identified as having a potential for hepatotoxicity, reported Alisa Likhitsup, MD, MPH, of the University of Michigan in Ann Arbor, and colleagues in an article in JAMA Network Open.
The six botanical supplements identified for their hepatotoxic potential were turmeric/curcumin–related, green tea extract, ashwagandha, Garcinia cambogia, red yeast rice, and black cohosh.
The estimated 15.6 million users is comparable to the number of U.S. patients prescribed potentially hepatotoxic medications such as simvastatin and nonsteroidal anti-inflammatory drugs, reported Likhitsup and her research team.
The researchers, however, wrote, “The safety and efficacy of herbal and dietary supplements remain inadequately established due to the absence of stringent regulatory mandates by the [FDA], which do not require human pharmacokinetic studies or prospective clinical trials before these products are brought to market.”
They also found an worrisome upward trend: cases of liver injuries blamed on herbal and dietary supplements rose from 7 percent in the 2004-2005 period to 20 percent during the study’s final two years in 2013-2014, according to the Drug-Induced Liver Injury Network, a multicenter observational study that collects data from U.S. patients with hepatotoxicity caused by various drugs and supplements. The Acute Liver Failure Study Group reported a similar upward trajectory for liver injury due to herbal and dietary supplements: from 12.4% in 1998-2007 to 21.1% in 2007-2015.
In the absence of regulatory scrutiny, loosely speaking, over botanical-product manufacturing and testing, as Likhitsup and her colleagues concluded, “to obtain a comprehensive history of medication and herbal and dietary supplement use when evaluating patients presenting with unexplained symptoms or abnormal liver test results” is recommended.
The most common uses cited by survey respondents for botanicals were “improving or maintaining health, preventing health issues, or enhancing immunity.”
The vast majority of users are intentionally using these products to self-treat or prevent a diagnosed or perceived medical condition, most frequently osteoarthritis, fatigue, or menopausal hot flashes,” said Maya Balakrishnan, MD, MPH, of Baylor College of Medicine in Houston, who was not involved with the study.
“The most striking thing is that most users are learning about and taking these botanicals independently, without discussion with their doctors,” Balakrishnan added.
It’s important for people to realize that most botanicals, when they’re taken as supplements, are concentrated far beyond what’s present in the botanical itself,” she said, emphasizing that clinicians need to have conversations about botanical products and their possible benefits and harms with patients.
“It means asking about herbal, botanical, and supplement use as part of the routine review of all medications,” she said.
For this study, Likhitsup and colleagues carried out a cross-sectional analysis with nationally representative data from NHANES, January 2017 to March 2020. They used population-estimates information from the 2020 U.S. Census.
For this cohort, the average age was 47.5 years for the 9,685 adult participants, where most of the respondents were women, and 62.2 percent were White, while 11.5 percent were Black, and 16.3 percent were Mexican or non-Mexican Hispanic.
Those using the six herbal and dietary supplements were significantly older, with adjusted OR 2.36 and 95% CI 1.06 to 5.25 for ages 40-59, and aOR 3.96 and 95% CI 1.93 to 8.11 for ages ≥60; higher educational attainment; and more likely to have had arthritis, with aOR 2.27 and 95% CI 1.62 to 3.29, P<0.001.
Of the users of turmeric, 26.8% reported using the product for joint health or arthritis. Amongst green tea users, the main reason cited by 27.2% was to enhance their energy level. For Garcinia cambogia, a statistically high percentage, 70%, of its users reported using the supplement for weight loss. A full 84.2% of black cohosh users were taking it to relieve hot flashes. The single most commonly stated reason for consuming red yeast rice was, at 90%, for heart health.
This article was originally published on medpagetoday Read the original article.
FAQs
What are some of the signs of liver damage due to botanical products?
Symptoms include weakness, nausea, jaundice, dark urine, and abdominal pain. If you have any of these symptoms seek medical advice immediately.
Do all herbal products cause hepatotoxicity?
No. Not all herbal products impart hepatotoxicity. It’s good to keep in mind, though, that researching each product, then consulting a healthcare provider before using the products would be quite advised.
How can I know if a product is safe?
Look for products that have been tested for safety and efficacy. Always read labels and consult credible sources of information about potential risks.
What if I think I have liver damage?
If you believe you have liver injury, discontinue using the product and seek medical evaluation by a healthcare provider with appropriate laboratory testing.
Is there a safer alternative to some of the more popular hepatotoxic botanicals?
Yes, there are safer alternatives. Now, consider herbal remedies with a lower risk profile or explore lifestyle changes that might bring similar benefits.